Podcast: Play in new window | Download
The Quadruple Aim of physician satisfaction is such an important aspect of value-based care. In the predominant world of fee-for-service reimbursement, physicians are struggling and burned out. Consequently, over half of all doctors won’t even recommend medicine as a career. This negative shift in wellbeing is important to understand because the attitudes and feelings of doctors bear directly on the way they treat patients. A recent Harvard report calls physician burnout “a public health crisis that urgently demands action.” Some physicians are even going as far as to say the profession is dealing with moral injury because the word “burnout” is insulting and insufficient in describing the pain they feel when the fee-for-service system prevents doctors from doing what’s right, thereby forcing them to inflict harm on patients – where physicians themselves experience a form of injury.
The business of fee-for-service medicine continues to get in the way of physicians healing patients. It breaks the spirit and the heart of our physician workforce, and it is imperative that physicians become empowered to lead a system transformation. Value-based care will be a losing effort if we do now cultivate physician wellbeing in the value journey.
In this podcast, you will hear from three physician thought leaders about the plight of physician burnout and its impact in advancing the aims of the value-based care movement. Most importantly, you will learn the tools necessary to transform organizational culture to ameliorate this important workforce challenge.
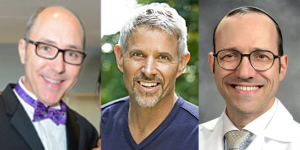
Speakers:
– Dike Drummond, M.D., CEO, Physician Coach & Speaker, TheHappyMD.com
– Moshe Cohn, M.D., Associate and Advisor, Moral Injury of Healthcare
– Amadeo Cabral, M.D., President, Turning Point Healthcare Consultants
Sponsored by: VBCExhibitHall.com (VBCEH)
 Episode Bookmarks:
Episode Bookmarks:
01:30 The differentiation between physician burnout and moral injury.
02:15 “Physicians need to heal in order to provide their best care for patients.”
03:00 Moral injury is a symptom of something larger – our broken health care system.
04:00 Introduction to Drs. Drummond, Cohn, and Cabral
05:45 Physician burnout and moral injury is a leadership failure.
06:30 Dr. Drummond provides context for why the physician workforce is suffering.
07:30 “The business of fee-for-service medicine gets in the way of physicians healing patients. It breaks our spirit and breaks our heart.”
07:45 “Burnout is a symptom of overwhelm in a physician that cares about what they do, when their purest expression of healer, helper, and light worker is blocked.”
08:15 Burnout is a physician impairment when it comes to ensuring quality and patient satisfaction.
08:45 Dr. Cohn explains the concept of why “language really matters” in communicating the public health crisis of physician burnout.
10:00 How physician moral injury is related to a clinical diagnosis of PTSD.
11:00 The leadership need for healthcare executives to address the repeated moral injury of their physician workforce.
12:30 How physician burnout differs from burnout we observe in other facets of the non-healthcare workforce.
13:15 The repeated barriers imposed by a system that prevents physicians in getting patients what they need to get better.
14:00 Dr. Cabral explains how the “slow boiling” public health emergency of physician burnout differs from more explosive public health emergencies like COVID-19.
15:00 Referencing confirmatory research (e.g. New York Times, Advisory Board) on the incongruence between the business of medicine and relationship-based care.
15:30 “Healthcare is not a broken “business” model — it is a broken “health care” model. It is imperative that physicians are at the table to lead a transformation.”
16:00 How do we get the incentives of business and medicine to merge into a congruent state?
17:30 The “canary in the coalmine” – physician suicides are signaling that something is wrong with the overall healthcare system.
18:00 An interesting dialogue about how Don Berwick posed an expansion to the Quadruple Aim as an apology for the Triple Aim.
19:00 Dr. Cabral on how true Value-Based Care (a wellness model) is a solution for physician wellbeing which can sometimes differ from the business model of VBC.
20:30 Dr. Cohn discusses the need a better definition for “Value” and why the Triple Aim does a disservice to the industry when the overall cost model is broken.
22:30 “As a physician, the only thing we really care about is patient outcomes. However, our outcomes are now mostly centered on checking boxes.”
24:20 Dr. Drummond reflects on the need for physicians to carve out a more rewarding practice in the reality of their business model.
24:45 Does capitation actually produce a healthier physician workplace with better patient outcomes?
26:30 The need for non-physician administrators to respect the healing encounter. (How many leaders regularly shadow their doctors?)
28:30 Dr. Cohn reflects on how investment levels prioritize societal importance (in relation to pediatrician compensation, mental health, education)
29:30 Dr. Cabral on how other countries are able to better align the incentives of their health care systems.
30:30 The physician burden of meeting end-of-life treatment expectations with heroic interventions that are costly (profitable) and result in poor quality of life.
31:45 The “classically American” problem of patients seeking low value care at end of life. (How does this factor into value-based care?)
32:45 “Eighty-percent of the hospital beds in our country are unnecessary if we granted our society the ability to determine what is a reasonable and unreasonable investment in quality of life.”
33:00 Dr. Cohn compares the current healthcare delivery system to a “fast food” model influenced by big money and advertising.
34:00 Advancements in technology and innovation in healthcare does not mean that we can fix everything that is wrong with patients.
36:15 Dr. Cabral discusses how patient satisfaction scores are being weaponized against providers.
37:30 The need for quality measures to translate into quality outcomes. (The misalignment leads to “check the box” medicine and weaponization against physicians.)
39:30 Dr. Cohn tells the painful story of a pediatric patient with a terminal brain bleed that led him to the realization of how administrators value documentation over human emotion.
41:30 Dr. Drummond explains how patient satisfaction should never be 100% (unless you are a criminal!)
42:00 “A true value journey requires a culture of provider support and a proactive burnout prevention strategy.”
42:30 The need for a super-majority value-based revenue tipping point in a contracting portfolio to bring about true cultural change.
43:45 Dr. Cabral on how the $4T American healthcare system spends 30% on administration (compared to 9-10% in other countries).
44:15 Healthcare Job Growth since 1970’s: 200% for providers and 3500% for non-clinical providers!
46:00 Drs. Cabral and Cohn speak about the monolithic structure of medical education that is over 100 years old and why that is a barrier to team-based care.
48:30 Dr. Drummond on how there are no leadership classes in medical school or residency (leadership is instead learned once practicing in a broken industry).
50:00 Dr. Drummond references Team Care Medicine, Dr. Jim Jerzak, and Dr. Corey Lyon as leading exemplars in team-based care models.
51:00 Dr. Cabral on how physicians “crossing the schism” into leadership often imposes unrealistic meeting expectations (unless the practice of medicine is completely abandoned).
52:45 Dr. Cohn on how healthcare leaders takes physicians for granted (referencing “The Daily Exploitation of Medical Staff” by Danielle Ofri)
54:00 Dr. Drummond – Should I go the extra mile for a patient if the organization gets in my way and it is unhealthy for me and my family?
55:30 Parting thoughts from our guests on implementing strategies to cultivate physician wellness.
